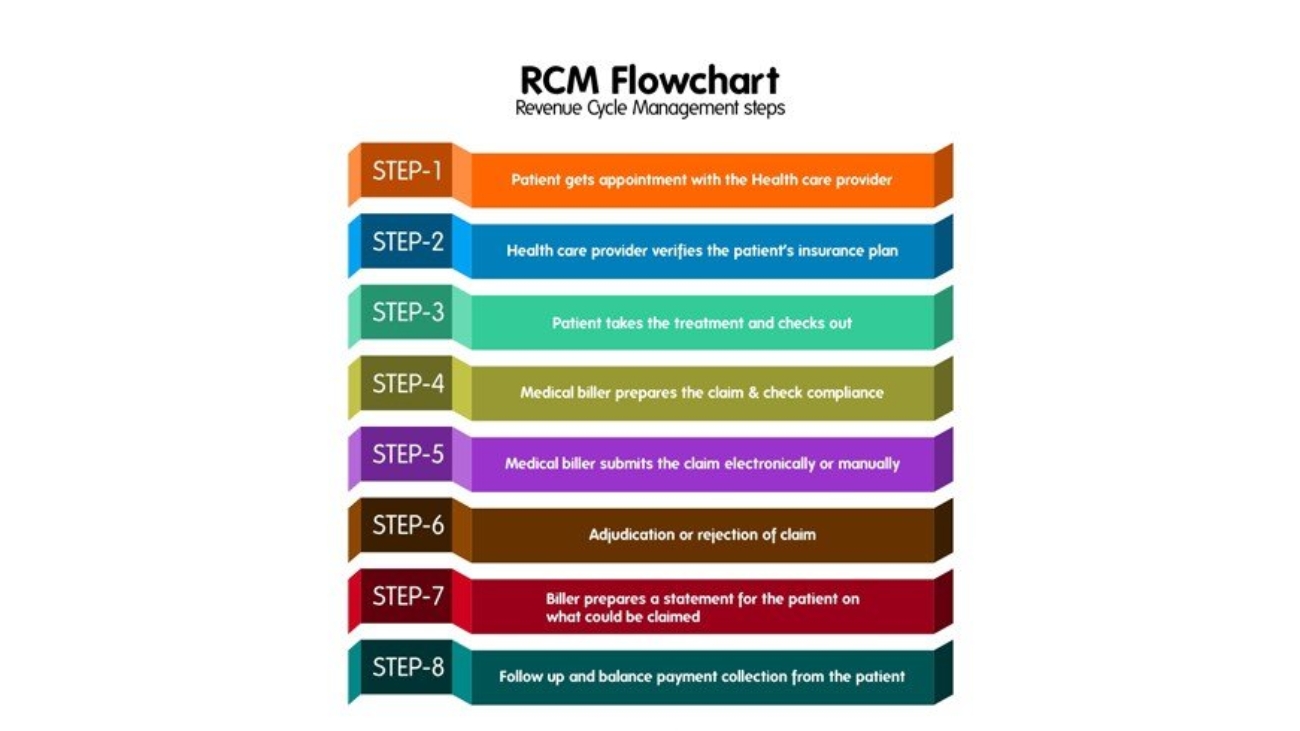
Beginner-Friendly Revenue Cycle Management Chart:
Revenue cycle management can be tricky to handle. But if you follow the right steps correctly, you can ensure timely reimbursements and improve the cash flow. These steps will prove to be beneficial if you are a beginner in managing billing and collections.
- Step 1:
The patient gets in touch with the healthcare organization or the clinic and books an appointment with the healthcare provider. Certain clinics use scheduling software while others do it manually.
- Step 2:
Patient eligibility verification is one of the most crucial steps of the revenue cycle management. The provider or the staff has to check whether the patient’s insurance plan covers the medical expenses. This step plays a vital role in the later part of the process.
- Step 3:
The providers complete the required medical procedures on the patient. The patient checks out while the provider passes on the health records to the billing team for the next steps.
- Step 4:
The billing team checks the health records and denotes the correct codes for every procedure performed. The claim is prepared according to the requirements of the patient’s insurance policy.
- Step 5:
The billing team submits the claims to the insurance network after doing rigorous checks for data in place. Though most payers accept electronic claims, some teams prefer to submit them manually.
- Step 6:
The insurance network checks the submitted claim. This takes up some time to complete. Meanwhile, the billing team has to follow up with the payer’s office frequently. Depending on the correctness of the submission, the claim is either accepted, denied due to certain errors or rejected altogether. As a medical biller, you have to make sure that the information on the claim is error-free and complete.
- Step 7:
Once the insurance payer reimburses a part of the claim, patients have to pay for the remaining balance amount. The billing team then prepares the complete bill for the patient explaining the insurance-coverage and the out-of-pocket expenditures.
- Step 8:
The last step is to collect the outstanding bill amount from the patient. However, laws like No Surprises Act have certain clauses on balance billing the patient. It is advisable that you keep yourself updated on them. Read the article here.