Being an orthopedic professional doesn’t seem so difficult, but in fact it is one of the toughest practices in the healthcare industry. Orthopedic coding falls in the second place while confronting the highest number of challenges in billing and coding for orthopedic procedures. Similarly, orthopedic coding team also faces challenges ranging from coding for common fractures to taking stock of bundling issues.
This article provides orthopedic coding professionals few handy tips to help them and their practice overcome four common orthopedic challenges and stay on track to deserved reimbursement this year. It’s also possible to make reimbursement rates stay constant without dropping down the rankings. Healthcare professionals must focus on the best ways to enhance their practices and develop their business in multiple areas.
Let’s have a look at 4 ways to overcome Orthopedic Coding Challenges:
- Castaway the fracture care coding confusion
- Know the updated descriptor for observation services
- Perfect Your Trigger Point Injection Claims
- Know Anatomy & Totality of Arthroplasty for Accurate Coding
1. Cast away the fracture care coding confusion
- More often, orthopedic professionals deal with fracture patients and report inaccurate codes related to fractures and their types. It can lead to revenue loss or claim denials.
- Hence, it’s even more crucial for them to stay updated and sharp when it comes to fracture care coding, and learning the intricacies involving terminology.
- One should know the difference between an open and closed fracture. It’s even more important to determine if the physician performed manipulation before selecting a fracture care code. They must prepare on the kinds of fractures required for physician manipulation.
- For instance, fractures that require manipulation include angulated, displaced, and dislocated. When healthcare professional finds any of these on the encounter forms, they should keep an eye out for evidence of manipulation.
2. Know the updated descriptor for observation services
- Reporting the healthcare professional’s observation services can be complicated if one is not able to pay attention.
- With two sets of codes to choose from, the codes chosen to use may depend on payer, length of stay, and many other factors that can make it tough to find the right or accurate code.
- However, CPT updates for 2021 have an update to one set of observation codes. When the hospitals report observation codes and overlook this E/M verbiage change, all of the descriptors add the phrase “outpatient hospital” in the phrase “outpatient hospital ‘observation status.”
3. Perfect Your Trigger Point Injection Claims
- It’s evident that patients in pain frequently require trigger point injections (TPIs) for their conditions. Even though these claims are reported with only two Trigger Point Injection codes, it ultimately doesn’t mean that reporting codes for TPIs are simple.
- For example, the covered or non-covered diagnoses for TPIs will vary by location, payer, and, on many occasions, encounter specifics.
- Most of the insurance companies will have limited payment policies for trigger point injections. So, be sure to check the policies that apply to the provided claims.
- Also, work with healthcare professionals to help match documentation to code requirements. For example, at times, they may need to go beyond the pain’s location and explain what has caused the pain.
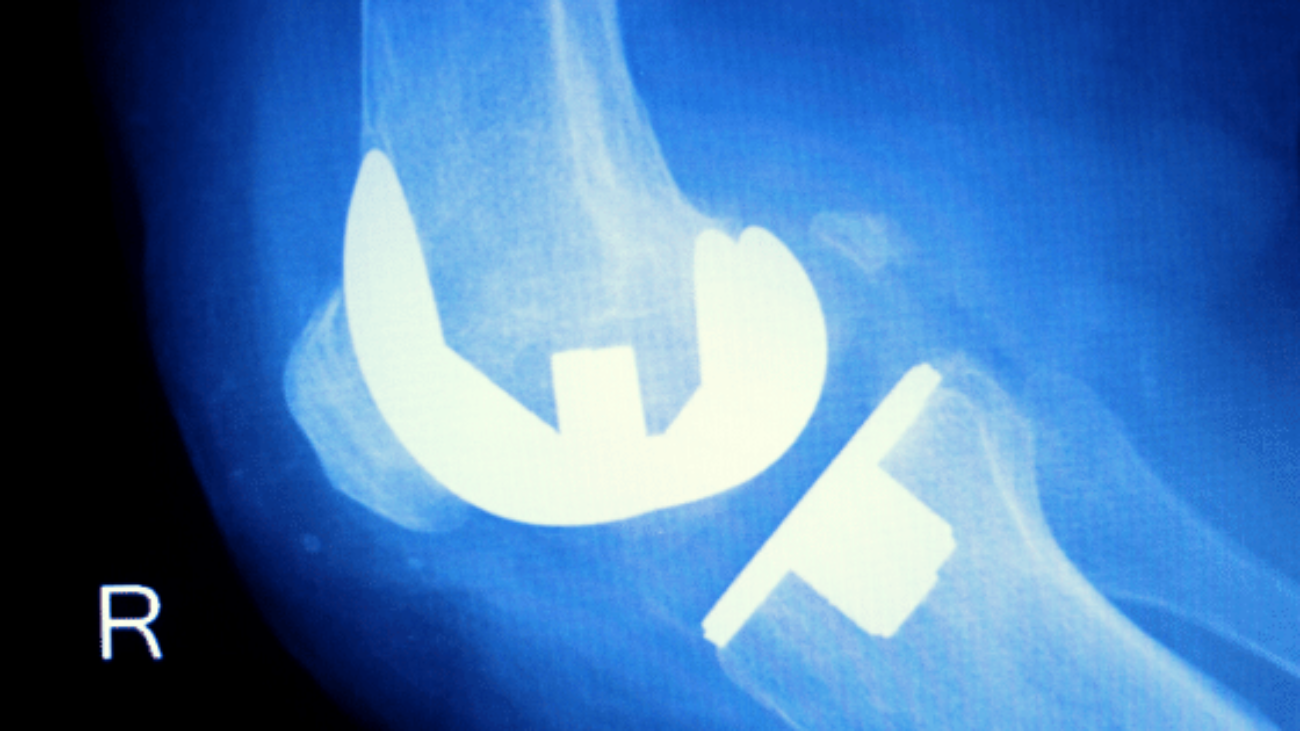
4. Know Anatomy & Totality of Arthroplasty for Accurate Coding
- In order to code a knee Arthroplasty properly, one should be aware of the anatomy and extent of the arthroplasty.
- When few arthroplasties are complete, few may only address some parts of the knee. Few common questions orthopedic coding teams might face while reporting knee arthroplasty procedures include:
- Is this a standard total knee replacement?
- Does the case involve both the femoral and tibial components?
- Does documentation meet payer policy and medical necessity requirements?
CMS CPT Codes 2021:
- Elements of CPT code changes include:
Retain five levels of coding for established patients
Reduce the number of levels to four for office/outpatient E/M visits for new patients
Revise the code definitions
Revise the times and medical decision-making process for all codes
Require performance of history and exam only as medically appropriate
Allow clinicians to choose the E/M visit level based on either Medical Decision Making or Time
CMS Documentation Guidelines 2021:
- Current rules and regulations for healthcare documentation list the documentation criteria as History, Examination, and/or Medical Decision Making.
- According to changes in 2021, a visit must be documented based on either Time or Medical Decision Making. Time criteria will be changed from “typical” to “minimum” and include both face-to-face and non-face-to-face. Face-to-face time will include examination and counseling and education, and non-face-to-face will include:
- Preparation to see patient-reviewing test results and obtained history
- Orders
- Documentation
- Care Coordination
- Medical Decision Making has been revised from its current state. Elements for coding choice have also been edited by removing ambiguous elements.
- The guidelines for Medical Decision Making were also interrupted further and moreover were reformatted. New definitions for data were implemented, and changes to risk were made. The three elements of Medical Decision Making include:
- Complexity of Problems
- Amount and/or Complexity of Data to be Reviewed and Analyzed
- Risk of Complications and/or Morbidity or Mortality of Patient Management
The other changes announced by CMS include:
- Accompanied by the above changes to the healthcare documentation process, CMS has announced other changes. They have adopted the AMA Specialty Society Relative Value Scale Update Committee, recommended values for the office/outpatient E/M visit codes for 2021, as well as the new add-on CPT code for prolonged service time.
- This particular change continues and will increase payment for office/outpatient E/M visits. There were more than 50 specialties that were surveyed in order to reach this decision.
- CMS also will be strengthening the Medicare-specific payment for office/outpatient E/M visits for primary care and non-procedural specialty care that were finalized in the 2019 PFS final rule.
Here are some facts to know about Orthopedic Coding:
- Back in 2013, the CPT manual had introduced various orthopedic coding changes and revisions. It had directly affected orthopedic reimbursements.
- There were almost 500 coding changes in Category I codes which made the process very complex.
- It was also accompanied by a complete overhaul of nerve conduction study codes. But now, two sets of new codes for shoulder and elbow revision were added along with a new spine fusion code.
- If you have multiple insurance companies, the worker’s compensation and personal injury liens can take you to inaccurate coding and denials or rejections, sometimes delays in reimbursements or payments.
- With an increase in patient number, the documentation requirements have also increased, which represents more time and effort from your staff to handle reimbursement collection.
- An increase in practice costs is another primary reason for worry. It can potentially cause disruptions in the cash flow of orthopedic practices.
- Though there are chances where these benefit orthopedic billing and coding procedures, you will need to keep in mind that your practices have minimal resources, which will hit the worst.
- Outsourcing billing and coding requirements may not put so much pressure on your work life. All these issues can be resolved with the extensive knowledge that outsourcing companies possess.
Even though there are various orthopedic coding changes involved, the healthcare professional must ensure to do better by outsourcing his/her service to a third party, which would be beneficial to both providers and patients.
Hope you got the required information on ways to overcome orthopedic coding challenges. For more queries and updates on healthcare, please subscribe to our blog. Do follow us on Facebook, LinkedIn, Twitter, and Instagram.