Updated: 20/02/2023
There is no one size fit for all and when you are looking to get the right mix of services and solutions a lot goes into making it work in tandem with regulatory practices and compliance. The importance of filing correct medical claims and the financial constraints that occur due to failure of doing so can pose a lot of problems to the revenue structure of hospitals and healthcare institutions. In contrast to other businesses, the administrative tasks in a healthcare facility are more difficult since clinical treatments, from the patient’s appointment to the account closure, are not necessarily shorter.
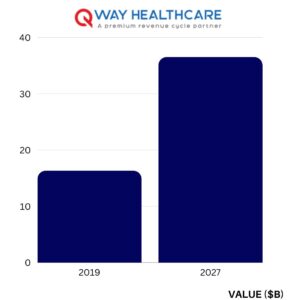
According to a leading research company, the global healthcare RCM outsourcing market was valued at USD 16.30 billion in 2019, and it is estimated to reach USD 36.51 billion by the end of 2027, delivering a CAGR of around 10.7% during the forecast period.
Tasks such as handling all the paperwork, determining eligibility, entering demographic information, billing and coding, and reporting medical claims are crucial to getting a clean claim and faster reimbursement. The claim will be disproved if even one step is omitted. So, with no strategic approach to optimize it, a fragmented revenue cycle management can result in a backlog of uncollectibles.
Let’s take dig into what are the parameters hospitals should look for while outsourcing billing services.
Related Post: Hospital Billing Services
1. Trained coders and billers:
A timely and correctly coded and billed claim will save the hospitals from facing the heat of heaps of pending claims. According to HIPAA mandates standardization of the medical codes, a regular compliance audit of the facility, electronic filing of medical claims, foolproof workstations, restricted access control to medical records and access only on a need basis, password-protected access to the software and online coding software is mandatory to be followed apart from trained coding and billing team.
As a healthcare provider, you must safeguard the privacy, security, and confidentiality of protected health information (PHI) by charging honestly and sticking to all the mandated protocols and guidelines of HIPPA. Claim appeal submission, bill changes, claim follow-up, and denial settlement will be handled by skilled teams who are educated about ICD-10 and ICD-11 coding. By doing this, you can keep a constant cash flow within your business, which will significantly improve your revenue cycle.
2. Accuracy and risk management:
To ensure revenue accuracy providers and hospitals should focus on demonstrating a commitment to manage value-based payments and shift towards value-driven solutions for patients. Improving internal processes, adjusting risk effectively, and providing quality care should be compounded for delivering end-to-end solutions to the hospitals by the revenue management companies.
Hospital billing companies should monitor processes to proactively identify issues that compromise revenue accuracy and take steps to mitigate risks thereby relieving the hospitals of claim denials. Once diagnostics have been documented, it is the responsibility of the billing company to ensure that no data is misplaced while it is carried through the various information systems.
3. Low A/R time:
Strategizing and focusing on low A/R days can be a game changer in hospital revenue processes and that is possible if the claim submission processes are optimized by integrating various metrics. Hospitals must ensure that billing companies are making efforts to ensure that the medical billing and coding process is accurately documented resulting in a decline in A/R days.
The quick execution of this vital step can be achieved by ensuring regular communication with physicians regarding unpaid receivables. Healthcare practitioners can quickly ascertain the status of various bills and payments with the use of medical billing and coding software.
Furthermore, when the primary EHR of a healthcare provider is integrated with the financial system, the results are optimized. As a result, the revenue cycle’s aspects are streamlined, ensuring the submission of legitimate claims.
4. Data-driven insights and analytics:
Healthcare billing companies can draw their expertise on moving towards a value-based reimbursement model rather than volume-based care. In the process, a large chunk of data related to patients can be accessed like electronic medical records, demographic values, and billing systems, among other health metrics and meaningful conclusions can be drawn upon data-driven decisions.
Hospital billing companies need to have a systematic approach and greater functionality for eligibility verification, processes for enhancing patient engagement, automating workflow for boosting interoperability, and honing skills through staff training.
Qway Healthcare Inc. can assist you in getting ready for the changes brought on by the healthcare industry and value-based reimbursements. Our qualified team can offer a glimpse into healthcare analytics and how you can use it to your advantage in your clinical settings because we leverage the most recent medical billing tools. Even the most seasoned specialists may find it difficult to understand these complicated requirements and constantly changing rules. Let’s simplify things for you.

