DME Billing & Coding Services
SpecialtyDME Billing & Coding Serv...
Durable Medical Equipment
Billing & Coding Services
DME billing refers to the process of billing for Durable Medical Equipment (DME) such as wheelchairs, hospital beds, and other medical devices. These bills are usually sent to third-party payers, such as insurance companies or Medicaid, for reimbursement.
The billing process involves identifying the DME item, determining the correct code to bill for it, verifying the patient’s insurance coverage, determining the appropriate amount to bill for the item, and submitting the bill to the payer.
Get A Free Quote
DME coding refers to the service of providing diagnostic medical equipment codes for use in electronic medical records, billing, and reimbursement purposes. These codes describe the type of diagnostic medical equipment used during medical procedures, its functionality, and its cost.
QWay’s DME Billing Process
-
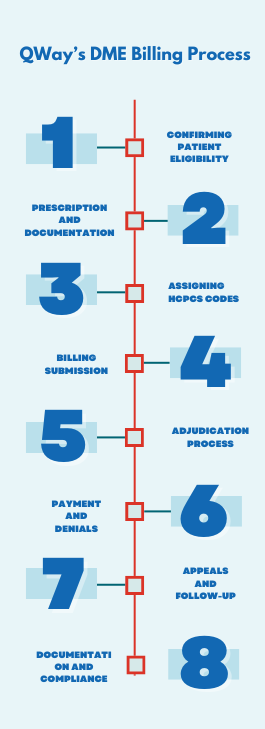 Confirming Patient Eligibility
Confirming Patient Eligibility
We start by verifying if the patient is eligible for DME coverage. This involves checking their insurance, ensuring they meet medical necessity criteria, and getting any necessary pre-authorization or referral.
- Prescription and Documentation
Once eligibility is confirmed, we collect a valid prescription from a licensed healthcare provider. The prescription should detail the type of equipment needed, quantity, duration of use, and any special instructions. We also gather all relevant patient documentation for billing purposes.
- Assigning HCPCS Codes
Each DME item is assigned a specific Healthcare Common Procedure Coding System (HCPCS) code. These codes help identify the equipment and facilitate billing. We choose the appropriate code based on the type of equipment, its features, and any additional accessories.
- Billing Submission
After the patient receives the DME, we submit a claim to their insurance company or payer. The claim includes the patient’s information, diagnosis code(s), HCPCS code(s) for the equipment, service dates, and any necessary supporting documents.
- Adjudication Process
The insurance company reviews the claim to ensure it meets coverage criteria and calculates the reimbursement amount. This process, known as adjudication, involves checking patient eligibility, coding accuracy, medical necessity, and coverage rules.
- Payment and Denials
If the claim is approved, we receive payment for the DME provided. Payment may be made directly to us or the patient if they paid out-of-pocket. If the claim is denied, we receive an explanation detailing the reasons for the denial.
- Appeals and Follow-Up
In case of denials or underpayments, we have the option to appeal the decision. This may involve providing additional documentation, correcting coding errors, or justifying the medical necessity of the DME. We follow up diligently to ensure prompt resolution of outstanding claims.
- Documentation and Compliance
Throughout the process, we maintain accurate documentation of patient encounters, prescriptions, claims, and communications with payers. Compliance with coding guidelines and regulations is crucial to minimize audit risks and penalties.
By following these steps, we ensure timely and accurate reimbursement for DME services while remaining compliant with regulations.
Challenges in DME Billing and Coding
The billing and coding of DME are complex and constantly evolving fields that necessitate ongoing education and an efficient billing process for timely claim payment. The challenges faced in DME billing and coding are;
DME billing is governed by intricate rules from entities like Medicare, Medicaid, and private insurers. Staying compliant with these rules amidst their constant changes is tough.
The HCPC System faces inefficiencies, leading to challenges in obtaining reimbursement for rendered services. These difficulties often stem from issues such as non-streamlined processes, incorrect application of modifiers, inadequate verification of payer and coding reports, and unclear documentation, contributing to obstacles in DME billing and coding reimbursement.
Dealing with payer contracts and meeting credential requirements can be time-consuming and bureaucratic. Failure to complete these processes accurately can lead to delays or denials of claims.
Implementing and managing billing software and EHR systems is challenging, especially for smaller DME providers with limited resources. Integration issues and software glitches can hinder billing processes.
Some DME items, such as custom orthotics or prosthetics, require intricate measurements, fittings, and customization for individual patients. Billing for these custom devices involves additional documentation and justification to meet payer requirements, adding complexity to the billing process.
Coverage policies for DME items can vary significantly among different regions and insurance plans. Navigating these discrepancies and ensuring compliance with specific coverage criteria for each patient’s location can be challenging, particularly for providers serving patients across multiple geographic areas.
DME services often require coordination among multiple healthcare providers, including physicians, therapists, and suppliers. Ensuring effective communication and collaboration among them to obtain necessary documentation and authorization can be challenging.
DME providers must manage inventory efficiently to meet patient demand while minimizing waste and excess costs. Balancing inventory levels with patient needs and reimbursement timelines requires careful monitoring and forecasting, which can be challenging in an unpredictable healthcare environment.
Proper utilization and maintenance of DME items are essential for patient outcomes and reimbursement eligibility. Educating patients about the use, care, and compliance requirements of DME products can be time-consuming and may require ongoing support to ensure optimal outcomes and reimbursement.
QWay’s Unique Approach in DME Billing & Coding
At QWay, our focus is on delivering specialized solutions in DME billing and coding that are uniquely crafted to suit your specific requirements. Here’s how we stand out;
- Firstly, our dedicated team of experts ensures precise and compliant billing resolutions for clients spanning all 50 states.
- Moreover, we strictly adhere to CMS and AMA guidelines, proficiently utilizing ICD-10-CM, and HCPCS coding standards.
- Additionally, by harnessing Electronic Health Records (EHR) systems, we advocate for top-tier clinical documentation, effectively reducing coding errors.
- Subsequently, to reduce denials in DME billing, we ensure thorough documentation, accurately code, verify insurance coverage, obtain necessary authorizations, stay updated with payer policies, and promptly address errors.
- Consequently, whether you’re an individual practitioner or part of a multi-specialty clinic/hospital, our tailored billing and coding services are designed to meet your unique needs.
- Nevertheless, we place a high priority on operational efficiency, ensuring minimal errors and maximum revenue generation.
- Moreover, we leverage various software solutions and customize our approach to align seamlessly with your DME billing requirements.
- In addition to our HBMA membership, we maintain strict compliance with HIPAA and ISO regulations.
- Lastly, our approach is characterized by a commitment to Quality, Quantity, and Quickness, supporting over 3500 providers in efficient revenue cycle management.
QWay: DME Billing Services Partner
Seeking a trustworthy and dependable partner for DME billing services? Our goal is to boost your revenue and simplify the processing of claims.
If you require assistance or have inquiries, feel free to reach out to us. We are dedicated to supporting you!