The healthcare sector is undergoing broad changes given the present scenario of the complex and competitive business environment. No wonder, we are seeing the rise in the number of medical billing companies trying to simplify the processes and making it easier for the healthcare service providers to increase the chances of effective reimbursements from the insurers and quick turnaround time concerning A/R.
But do you wonder what impact your revenue cycle will face if your medical billing service provider is not doing enough to help you with the tedious processes involved in streamlining the steps about insurance companies and claims requests? Given the substantial amount of work involved in claiming the amount from insurance companies there are a lot of things to check before choosing RCM healthcare provider.
The weathering effects of increasing costs and poor governance on expenses incurred along with slow processes of claims reimbursement has proved to be a whole new set of challenging issues that have to be tackled for maximization of claim amounts.
|“Eighty-seven percent of healthcare executives agree that their organization’s business and technology strategies are becoming inseparable—even indistinguishable.” Source Accenture Insights |
Let us dive into pain points that may occur if we don’t scrutinize the healthcare billing provider and end up not selecting the right one:
Poor Focus on Patient Care:
If the healthcare providers are continuously bogged down with managing loopholes of complicated billing dynamics and tedious documentation work their energies will be drained dealing with these issues which can be easily solved had they invested more time in selecting the right healthcare billing company.
A billing company can be an energy vampire for healthcare providers if certain parameters are not met and checked. With all the concentration on dealing with these issues, the focus on patient care will be less resulting in loss of revenue and pulverization of the organization’s or individual providers’ reputation.
Billing Errors:
One of the most important and complex steps to comprehend is billing as since the start of the medical encounter every step has to be billed and documented well to avoid complications in claiming the reimbursement from the insurers. Inefficiency on the part of billing companies may lead to higher claim rejections and lower reimbursement rates.
Being well-versed with industry nuances and being up to date with the domain-specific knowledge and standards will help a billing company go a long way with the healthcare providers in giving them accurate specifications and service delivery thus leading to a reduction in billing errors.
Don’t forget to check whether the company is complying with various industry standards and is ISO and HIPAA certified to ensure that the sensitive patient data and personal health information is secured and won’t go into the wrong hands.
Related: 10 Steps to Choose the Right Medical Billing and Coding Companies
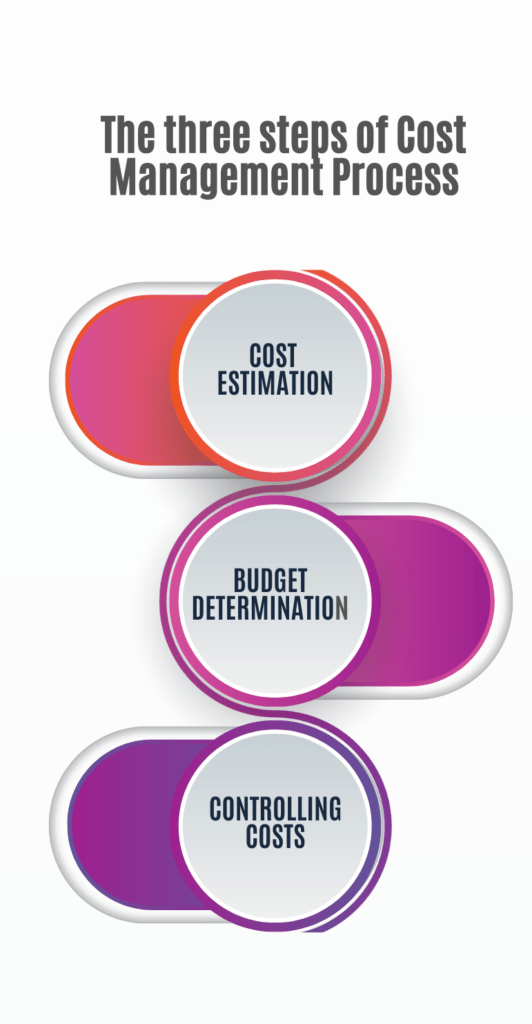
Cost Governance:
If you wish to architect your company’s financial environment in a structured way then monitoring costs becomes a major factor. Harnessing the power of effective cost management can help you save from facing budget overruns.
Billing companies with faulty processes and inexperienced teams might not be able to give you complete insights into usage tracking and keeping a tab on incurred costs leading to disruption of budgets allocated. Effective cost governance includes monitoring cost performance, ensuring all changes are noted and submitted, and communicating the impact of the changes to healthcare providers.
Cost governance can be a competitive advantage that will help to track everything down resulting in a better revenue management cycle and accelerated cash flows.
Coding Errors:
Every service to be calculated for revenue generation has to be coded first according to its Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System codes and then the claims are submitted to the insurers for reimbursements. Coding errors result in denial of claims and the same reflects in patient care quality.
If the billing company hasn’t trained its teams with regards to complying with the standards and coding procedures your revenue health is going to suffer subsequently also amounting to heaps of paperwork for re-submission of the claims and stressful tasks for removing the errors.
The consequences of miscoding and submitting incorrect claims can result in huge sums of penalty charges and if the fraud involves Medicare or Medicaid then civil penalties for violating the civil FCA may include recovery of up to three times the amount of damages sustained by the Government as a result of the false claims, plus financial penalties per false claim filed.
(*) All the unnecessary ruckus can be avoided if the medical billing teams are keeping themselves updated with the latest changes in codes and standards and are documenting the claims accurately leaving no space for loss of revenue.
Medical billing outsourcing and coding services serve as a support to the healthcare providers helping them to focus on core functions of their business operations and aim at improving overall patient care. To avoid losing on the influx of revenue the selection of the right medical billing outsourcing companies is a must for harboring deep and prolonged client satisfaction.